Deadly Fungi: The Emerging Superbug Crisis
Table of Contents
The Rise of Antifungal Resistance
The effectiveness of our fight against deadly fungi is hampered by the growing problem of antifungal resistance. Similar to antibiotic resistance in bacteria, fungi are developing mechanisms to evade the effects of antifungal drugs, rendering treatments ineffective. This drug resistance is a complex issue with multiple contributing factors.
-
Overuse of broad-spectrum antifungals in agriculture: The widespread use of azoles and other antifungals in agriculture to protect crops from fungal diseases has inadvertently created selective pressure, leading to the evolution of resistant strains. These resistant strains can then spread to humans through the food chain or the environment.
-
Inappropriate prescribing practices in healthcare settings: Over-prescription or the use of broad-spectrum antifungals when narrower-spectrum drugs would suffice contributes significantly to antifungal resistance. This is further exacerbated by a lack of proper diagnostic testing, often resulting in unnecessary antifungal treatments.
-
Lack of new antifungal drug development: The pharmaceutical industry has historically underinvested in the development of new antifungal drugs, leading to a limited arsenal of effective treatments. This scarcity of new options accelerates the selection and spread of resistant strains.
-
Genetic mutations leading to drug resistance in fungi: Fungi, like bacteria, can develop genetic mutations that alter their cellular mechanisms, rendering them resistant to specific antifungal agents, such as azoles, echinocandins, and polyenes.
-
The spread of resistant strains through healthcare facilities and communities: Resistant strains of fungi, such as Candida auris, can easily spread in healthcare settings, particularly among immunocompromised individuals. This rapid transmission necessitates robust infection control measures.
High-Risk Populations and Deadly Fungal Infections
Certain populations are significantly more susceptible to severe and potentially fatal fungal infections. These individuals often have weakened immune systems, making them vulnerable to opportunistic fungal pathogens.
-
Patients undergoing chemotherapy or radiation therapy: Cancer treatments often suppress the immune system, leaving patients highly susceptible to deadly fungal infections.
-
Individuals with HIV/AIDS: HIV weakens the immune system, increasing the risk of serious fungal infections such as cryptococcosis and candidiasis.
-
Organ transplant recipients taking immunosuppressants: Immunosuppressive drugs, necessary to prevent organ rejection, also increase susceptibility to fungal infections.
-
Neonates and infants: Newborns and infants have immature immune systems, making them vulnerable to invasive fungal diseases.
-
Individuals with chronic lung diseases: Conditions like cystic fibrosis and chronic obstructive pulmonary disease (COPD) can increase the risk of developing aspergillosis and other lung-based fungal infections.
Specific deadly fungal infections like Candida auris, Aspergillus, and Cryptococcus pose severe threats. Candida auris, for example, is particularly concerning due to its high mortality rate and multi-drug resistance. Invasive aspergillosis can be fatal if left untreated, while cryptococcosis frequently affects individuals with compromised immune systems, causing meningitis and other life-threatening complications. Mucormycosis, while less common, is also a devastating and often fatal fungal infection, particularly affecting individuals with diabetes or weakened immune systems.
The Challenges of Diagnosing and Treating Deadly Fungal Infections
Diagnosing deadly fungal infections can be challenging due to several factors:
-
Difficulties in differentiating fungal infections from bacterial infections: The symptoms of fungal and bacterial infections can overlap, leading to misdiagnosis and delays in appropriate treatment.
-
Slow growth of some fungal species in culture, delaying diagnosis: Traditional diagnostic methods relying on fungal cultures can be time-consuming, delaying the initiation of appropriate treatment.
-
Lack of rapid and sensitive diagnostic tests for many fungal infections: The development of rapid diagnostic tests is crucial for timely diagnosis and improved patient outcomes.
Treatment options for invasive fungal infections are also limited:
-
Limited availability of effective antifungal drugs: The number of antifungal drugs available is far fewer than antibacterial agents, and the existing drugs often have significant side effects.
-
Emergence of resistance to currently available antifungal agents: The increasing prevalence of antifungal resistance further complicates treatment and necessitates the development of novel therapeutic strategies.
Prevention and Control Strategies for Deadly Fungi
Combating the threat of deadly fungi requires a multifaceted approach incorporating prevention and control strategies:
-
Strict adherence to hand hygiene protocols: Basic hygiene practices are crucial in preventing the spread of fungal pathogens, especially in healthcare settings.
-
Environmental cleaning and disinfection in healthcare facilities: Regular cleaning and disinfection of healthcare environments can help reduce the risk of fungal contamination.
-
Responsible use of antifungals to minimize resistance: Prudent use of antifungal medications is essential to slow the development of resistance.
-
Development of rapid diagnostic tests: Rapid diagnostic tools are crucial for early detection and appropriate treatment.
-
Research and development of novel antifungal therapies and vaccines: Significant investment in research is needed to develop new antifungal drugs and vaccines to combat resistant strains.
-
Improved surveillance systems to track the spread of resistant fungi: Robust surveillance systems are essential to monitor the emergence and spread of resistant fungal pathogens. This data is crucial for guiding public health responses.
Conclusion
The emergence of deadly fungi as a superbug crisis presents a significant global health threat. Antifungal resistance, coupled with challenges in diagnosis and treatment, necessitates urgent action. We must prioritize research into new antifungal drugs, implement stringent infection control measures, and improve diagnostic capabilities to combat this escalating crisis of deadly fungi. Increased awareness and understanding of this emerging threat are crucial to protecting vulnerable populations and mitigating the spread of these dangerous pathogens. Learn more about the fight against deadly fungi and how you can contribute to prevention efforts. Let's work together to prevent the further spread of these dangerous and increasingly resistant organisms.
Featured Posts
-
 Kripto Duezenlemelerinde Yeni Bir Cag Spk Nin Etkisi
May 08, 2025
Kripto Duezenlemelerinde Yeni Bir Cag Spk Nin Etkisi
May 08, 2025 -
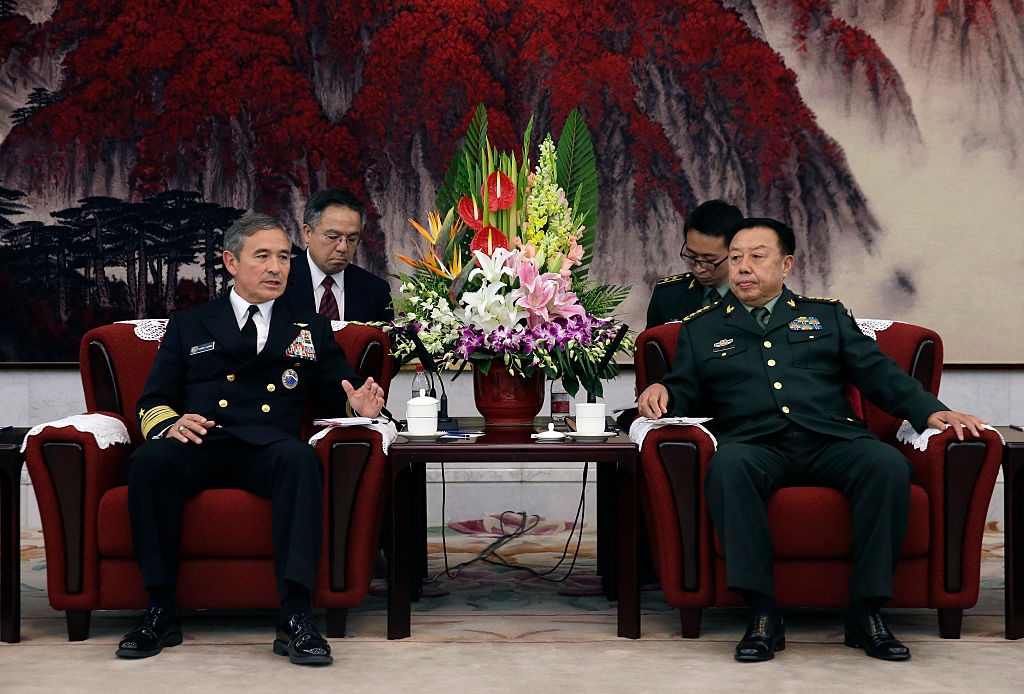 High Level U S And Chinese Officials To Discuss Trade War Resolution
May 08, 2025
High Level U S And Chinese Officials To Discuss Trade War Resolution
May 08, 2025 -
 Confirmado Neymar Vuelve A La Seleccion Y Jugara Contra Messi En El Monumental
May 08, 2025
Confirmado Neymar Vuelve A La Seleccion Y Jugara Contra Messi En El Monumental
May 08, 2025 -
 Arsenal Vs Ps Zh Pregled Pred Natprevarot Od Ligata Na Shampionite
May 08, 2025
Arsenal Vs Ps Zh Pregled Pred Natprevarot Od Ligata Na Shampionite
May 08, 2025 -
 New Uber Subscription What Drivers Need To Know
May 08, 2025
New Uber Subscription What Drivers Need To Know
May 08, 2025
