Fungal Infections: A Growing Threat Of Antibiotic Resistance
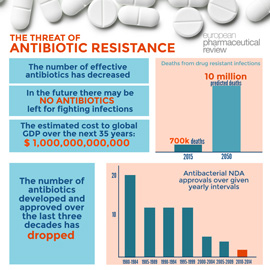
Table of Contents
The Increasing Prevalence of Fungal Infections
The incidence of fungal infections is rising globally, posing a significant challenge to healthcare systems worldwide. This increase is driven by several interconnected factors.
Factors Contributing to Increased Prevalence
-
Aging Population: As the global population ages, the number of individuals susceptible to opportunistic fungal infections, such as Candida and Aspergillus, is dramatically increasing. Elderly individuals often have weakened immune systems, making them more vulnerable.
-
Immunocompromised Individuals: Individuals with compromised immune systems, including those with HIV/AIDS, cancer, organ transplants, or those undergoing chemotherapy, are at significantly higher risk of developing serious fungal infections. These infections can be life-threatening if not treated promptly and effectively.
-
Increased Use of Broad-Spectrum Antibiotics: The overuse and misuse of broad-spectrum antibiotics disrupt the delicate balance of the gut microbiome, leading to an overgrowth of opportunistic fungi like Candida albicans. This creates a fertile ground for fungal infections to take hold.
-
Climate Change: Changing climate patterns are expanding the geographical range of many fungal species, leading to increased human exposure and the emergence of novel fungal pathogens.
-
Global Travel and Migration: Increased global travel and migration facilitate the rapid spread of drug-resistant fungal strains across geographical boundaries, making containment challenging.
-
Bullet Points:
- The global burden of fungal infections is estimated to be millions of cases annually, with a substantial number resulting in mortality.
- Common fungal infections include candidiasis (caused by Candida species), aspergillosis (caused by Aspergillus species), and cryptococcosis (caused by Cryptococcus species). These infections can manifest in various forms, from superficial skin infections to life-threatening invasive diseases.
- High-risk populations include individuals with weakened immune systems, those receiving prolonged antibiotic therapy, and those with underlying medical conditions such as diabetes and chronic lung disease.
The Mechanisms of Antifungal Resistance
The development of antifungal resistance mirrors the mechanisms observed in bacterial antibiotic resistance. Fungi employ several strategies to evade the effects of antifungal drugs.
How Fungi Develop Resistance
-
Mutations in Target Genes: Fungi can develop mutations in the genes encoding the target sites of antifungal drugs, rendering the drugs ineffective. This is a common mechanism for resistance development.
-
Efflux Pumps: Many fungi possess efflux pumps, which actively transport antifungal drugs out of the fungal cell, reducing intracellular drug concentrations and preventing their effect.
-
Target Modification: Fungi can modify the target site of the antifungal drug, reducing its binding affinity and minimizing its inhibitory effect. This can involve alterations in the fungal cell wall or membrane.
-
Enzyme Production: Some fungi produce enzymes that can degrade or modify antifungal drugs, inactivating them before they can reach their target.
-
Bullet Points:
- Azoles, echinocandins, and polyenes are common classes of antifungal drugs, each facing specific resistance mechanisms.
- Resistance to azoles, for example, often arises from mutations in the CYP51A1 gene, which encodes a crucial enzyme involved in ergosterol biosynthesis.
- The genetic basis of antifungal resistance is complex and involves multiple genes and regulatory pathways.
The Impact of Antifungal Resistance on Healthcare
Antifungal resistance significantly impacts healthcare systems, leading to a range of challenges in diagnosis, treatment, and management of fungal infections.
Challenges in Treatment and Management
-
Increased Treatment Failure Rates and Prolonged Hospital Stays: Treatment failure rates are significantly higher for infections caused by resistant fungal strains, leading to prolonged hospital stays and increased healthcare costs.
-
Higher Mortality Rates in Severe Infections: Resistant fungal infections are associated with significantly higher mortality rates, particularly in immunocompromised individuals.
-
Limited Availability of Effective Antifungal Therapies: The pipeline for new antifungal drug development is limited, leaving clinicians with fewer options for treating resistant infections.
-
Increased Healthcare Costs: Managing resistant fungal infections is considerably more expensive than treating susceptible infections, due to prolonged hospital stays, the use of more expensive drugs, and the need for more intensive care.
-
Bullet Points:
- Mortality rates for invasive candidiasis caused by resistant strains can exceed 50%.
- The economic burden of antifungal resistance is substantial, placing a significant strain on healthcare budgets globally.
- Early diagnosis and rapid initiation of appropriate antifungal therapy are crucial in improving outcomes.
Strategies to Combat Antifungal Resistance
Combating antifungal resistance requires a multi-pronged approach involving prevention, improved diagnostics, and the development of new therapies.
Preventing the Spread of Resistance
-
Improved Infection Control Practices: Strict infection control measures in healthcare settings are essential to minimize the transmission of resistant fungi. This includes hand hygiene, appropriate use of personal protective equipment, and environmental decontamination.
-
Responsible Use of Antifungal Medications: Prescribing antifungals only when necessary, adhering to recommended treatment regimens, and avoiding unnecessary prophylaxis are critical steps in preventing the development and spread of resistance.
-
Development of New Antifungal Drugs and Therapies: Intensified research and development efforts are urgently needed to discover and develop novel antifungal agents targeting different pathways in fungal cells.
-
Surveillance and Monitoring of Antifungal Resistance: Robust surveillance systems are necessary to track the emergence and spread of resistant strains, enabling timely intervention and the implementation of targeted control measures.
-
Bullet Points:
- Public health initiatives play a crucial role in educating healthcare professionals and the public about the risks of antifungal resistance.
- Ongoing research focuses on exploring novel drug targets and developing new classes of antifungal agents.
- Patient education is essential in promoting responsible use of antifungal medications and improving adherence to treatment regimens.
Conclusion
The rise of antifungal resistance poses a significant and growing threat to global health, demanding urgent and concerted action. The increasing prevalence of fungal infections, coupled with the emergence of drug-resistant strains, necessitates a comprehensive strategy. This strategy must include responsible antifungal stewardship, improved infection control, accelerated research and development of new therapies, and enhanced surveillance systems. We must proactively combat this threat to ensure the effective treatment of fungal infections and prevent further escalation of antifungal resistance. Understanding the risks associated with antifungal resistance is crucial in safeguarding public health. Let’s work together to address this challenge and prevent the further spread of resistant fungal infections.
Featured Posts
-
 The Night Counting Crows Changed Their Destiny On Saturday Night Live
May 08, 2025
The Night Counting Crows Changed Their Destiny On Saturday Night Live
May 08, 2025 -
 Counting Crows 1995 Snl Performance A Retrospective
May 08, 2025
Counting Crows 1995 Snl Performance A Retrospective
May 08, 2025 -
 Caruso Makes Nba Playoff History Thunder Game 1 Win
May 08, 2025
Caruso Makes Nba Playoff History Thunder Game 1 Win
May 08, 2025 -
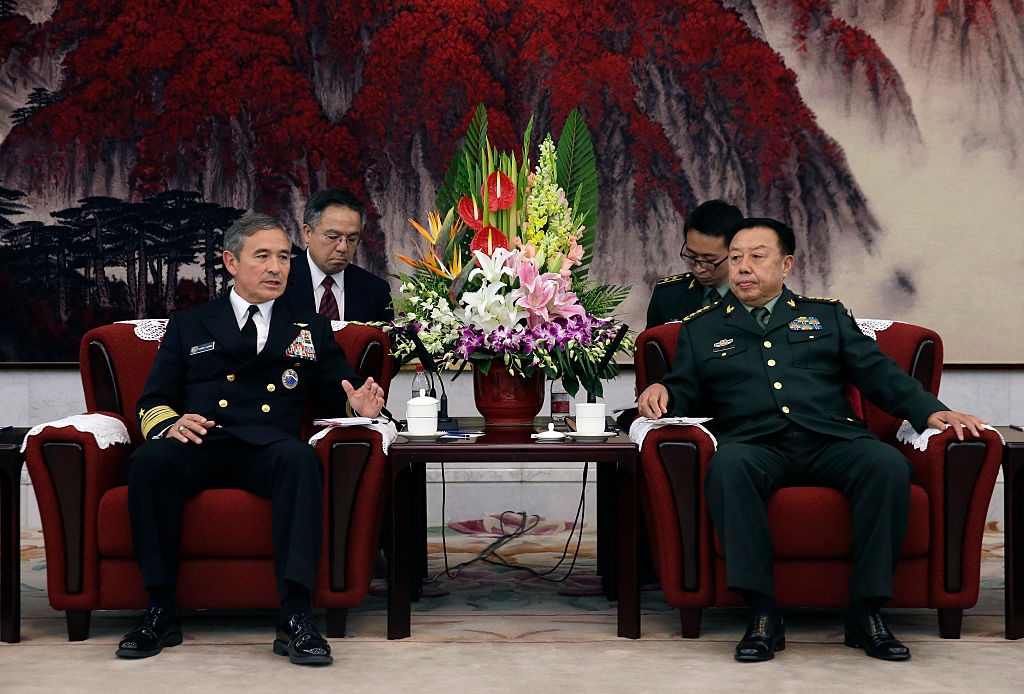 High Level U S And Chinese Officials To Discuss Trade War Resolution
May 08, 2025
High Level U S And Chinese Officials To Discuss Trade War Resolution
May 08, 2025 -
 Us Canada Trade Talks A Path Towards Coherence
May 08, 2025
Us Canada Trade Talks A Path Towards Coherence
May 08, 2025
