Ghana's Mental Healthcare System: 80 Psychiatrists For 30 Million People

Table of Contents
The Stark Reality: A Critical Shortage of Mental Health Professionals
Ghana suffers from a profound shortage of mental health professionals. The scarcity extends beyond psychiatrists; psychologists, psychiatric nurses, and other crucial mental health workers are also in critically short supply.
- The Numbers: While the exact figures fluctuate, estimates consistently reveal a devastating gap. The ratio of psychiatrists to population is far below the World Health Organization's recommended levels. Similar shortages exist for other mental health professionals, leaving a vast unmet need.
- International Comparison: Compared to other African nations and global averages, Ghana’s mental health professional-to-population ratio is alarmingly low, highlighting the urgency of the situation. Many countries with comparable populations have significantly more mental health professionals per capita.
- Brain Drain: The limited opportunities and low compensation for mental health professionals in Ghana lead to a significant brain drain. Skilled professionals often seek better prospects abroad, exacerbating the existing shortage within the country.
- Impact on Access: This critical shortage directly impacts access to care. Long waiting lists, limited appointment availability, and geographical barriers further hinder individuals seeking help.
Limited Access to Mental Healthcare Services: Geographical and Socioeconomic Barriers
Accessing mental healthcare in Ghana presents significant geographical and socioeconomic obstacles. These barriers disproportionately affect vulnerable populations, exacerbating the mental health crisis.
- Geographical Challenges: Rural communities often lack access to mental health services, with limited transportation options and long distances to the nearest facilities posing significant hurdles. Many rural areas have no mental health professionals at all.
- Socioeconomic Barriers: The cost of treatment, including consultations, medication, and therapy, places an insurmountable burden on many Ghanaians, particularly those in lower socioeconomic groups. Furthermore, the stigma surrounding mental illness prevents many from seeking help, even if services are available.
- Help-Seeking Behavior: The combined effect of these barriers significantly impacts help-seeking behaviour. Many individuals suffering from mental illness remain untreated, leading to worsening conditions and potentially tragic consequences.
- Disproportionate Impact: Marginalized groups, including women, children, and people with disabilities, are disproportionately affected by these limited access issues.
The Stigma Surrounding Mental Illness in Ghana: A Major Obstacle to Seeking Help
Deep-rooted cultural beliefs and societal attitudes contribute significantly to the stigma surrounding mental illness in Ghana. This stigma acts as a powerful barrier to seeking help and accessing treatment.
- Cultural Beliefs: Traditional beliefs often attribute mental illness to supernatural causes, leading to misconceptions and fear. This fuels stigma and prevents individuals from seeking professional help, often opting for traditional healers instead.
- Consequences of Untreated Illness: The stigma surrounding mental illness in Ghana leads to delayed treatment, preventing early intervention and contributing to worsening symptoms and potentially severe consequences. Many individuals suffer in silence, afraid of judgment and social exclusion.
- Impact on Help-Seeking: Fear of social isolation, discrimination, and family rejection prevents many from disclosing their mental health struggles and seeking professional help. This silence further perpetuates the cycle of stigma and untreated illness.
- Successful Initiatives: Despite the challenges, several initiatives are underway to destigmatize mental illness in Ghana. These include public awareness campaigns, educational programs, and community-based support groups.
Inadequate Funding and Infrastructure: Hampering the Development of Mental Healthcare
Insufficient funding and inadequate infrastructure significantly hinder the development of a comprehensive and effective mental healthcare system in Ghana.
- Insufficient Funding: Government allocation for mental healthcare remains drastically low compared to other healthcare sectors. This lack of funding impacts staffing, training, facility development, and the provision of essential services.
- Lack of Infrastructure: Many regions lack adequate mental health facilities, including hospitals, community-based centers, and rehabilitation programs. The existing infrastructure is often outdated and under-resourced.
- Impact on Quality of Care: Inadequate funding and infrastructure directly affect the quality of care provided. Limited resources restrict access to essential medications, therapies, and support services.
- Policy Gaps: The absence of a comprehensive and well-funded national mental health policy further exacerbates the challenges faced by the system.
Government Initiatives and Ongoing Efforts to Improve Mental Healthcare
The Ghanaian government has initiated several programs and policies to address the mental health crisis. While these efforts are commendable, significant improvements are still needed.
- Current Initiatives: The government has implemented various mental health programs, including training initiatives for healthcare professionals, community-based mental health services, and public awareness campaigns.
- Policy Effectiveness: The effectiveness of current mental health policies needs evaluation and strengthening to ensure alignment with the needs of the population.
- Successful Programs: Certain community-based programs have shown success in providing accessible mental health services, highlighting the potential for scaling up such initiatives.
- Areas for Improvement: Increased funding, strengthened infrastructure, improved professional training, and more effective integration of mental health into the broader healthcare system are crucial.
The Role of NGOs and Community-Based Organizations in Providing Mental Healthcare
Non-governmental organizations (NGOs) and community-based organizations play a vital role in filling the gaps in Ghana's mental healthcare system.
- NGO Contributions: NGOs provide essential mental health services, including counseling, support groups, and community outreach programs, often reaching marginalized communities neglected by the formal healthcare system.
- Successful Community Initiatives: Many community-based initiatives have demonstrated success in providing culturally sensitive and accessible mental health services.
- Challenges Faced: NGOs often face funding constraints, capacity limitations, and challenges in scaling up their operations to meet the overwhelming needs.
- Collaboration: Effective collaboration between government agencies and NGOs is crucial for a more comprehensive and sustainable approach to mental healthcare.
The Path Forward: Recommendations for Improving Ghana's Mental Healthcare System
Transforming Ghana's mental healthcare system requires a multi-pronged approach involving increased investment, policy reform, and community engagement.
- Improved Access: Expanding access to mental healthcare services, particularly in rural areas, is paramount. This includes establishing more facilities, training community health workers, and utilizing mobile clinics.
- Addressing the Shortage: Investing heavily in training and retaining mental health professionals is crucial. This requires improved salaries, better working conditions, and opportunities for professional development.
- Reducing Stigma: Widespread public awareness campaigns are needed to challenge stigma and promote help-seeking behavior. Education on mental health should be integrated into school curricula and community programs.
- Increased Funding and Infrastructure: Substantial increases in government funding are essential to improve infrastructure, train personnel, and provide quality mental health services.
The Importance of Mental Health Awareness and Education
Raising mental health awareness and promoting mental health literacy are critical for improving the overall well-being of the Ghanaian population.
- Public Education Campaigns: Sustained public education campaigns are crucial to disseminate accurate information about mental illness, dispelling myths and misconceptions.
- Mental Health Education in Schools and Communities: Integrating mental health education into school curricula and community programs helps to destigmatize mental illness and promotes help-seeking behavior.
- Improved Mental Health Literacy: Improving mental health literacy equips individuals with the knowledge and skills to recognize, understand, and respond appropriately to mental health challenges.
- Promoting Mental Health Education: Investing in training teachers, community leaders, and healthcare workers to deliver effective mental health education is essential.
Conclusion
Ghana's mental healthcare system faces immense challenges, primarily the critical shortage of mental health professionals and limited access to services compounded by stigma and inadequate funding. However, ongoing government initiatives and the vital role played by NGOs offer a glimmer of hope. To truly improve Ghana's mental healthcare, substantial investment in training and retaining professionals, infrastructure development, and public awareness campaigns is crucial. We must work together to overcome the stigma surrounding mental illness and ensure that every Ghanaian has access to quality mental health services. Improve Ghana's mental healthcare system by supporting mental health initiatives in Ghana, advocating for better mental health access in Ghana, and learning more about Ghana's mental health crisis. Let's work towards a Ghana where mental well-being is prioritized and every individual has the support they need.

Featured Posts
-
 Massive Office 365 Data Breach Results In Millions In Losses
May 03, 2025
Massive Office 365 Data Breach Results In Millions In Losses
May 03, 2025 -
 Sydney Harbour Surveillance Heightened Amidst Rise In Chinese Ship Sightings
May 03, 2025
Sydney Harbour Surveillance Heightened Amidst Rise In Chinese Ship Sightings
May 03, 2025 -
 Avrupa Ile Is Birligimizi Gueclendirecegiz Son Dakika Gelismeleri
May 03, 2025
Avrupa Ile Is Birligimizi Gueclendirecegiz Son Dakika Gelismeleri
May 03, 2025 -
 Christina Aguileras Altered Image A Look At The Fan Reaction To Recent Photos
May 03, 2025
Christina Aguileras Altered Image A Look At The Fan Reaction To Recent Photos
May 03, 2025 -
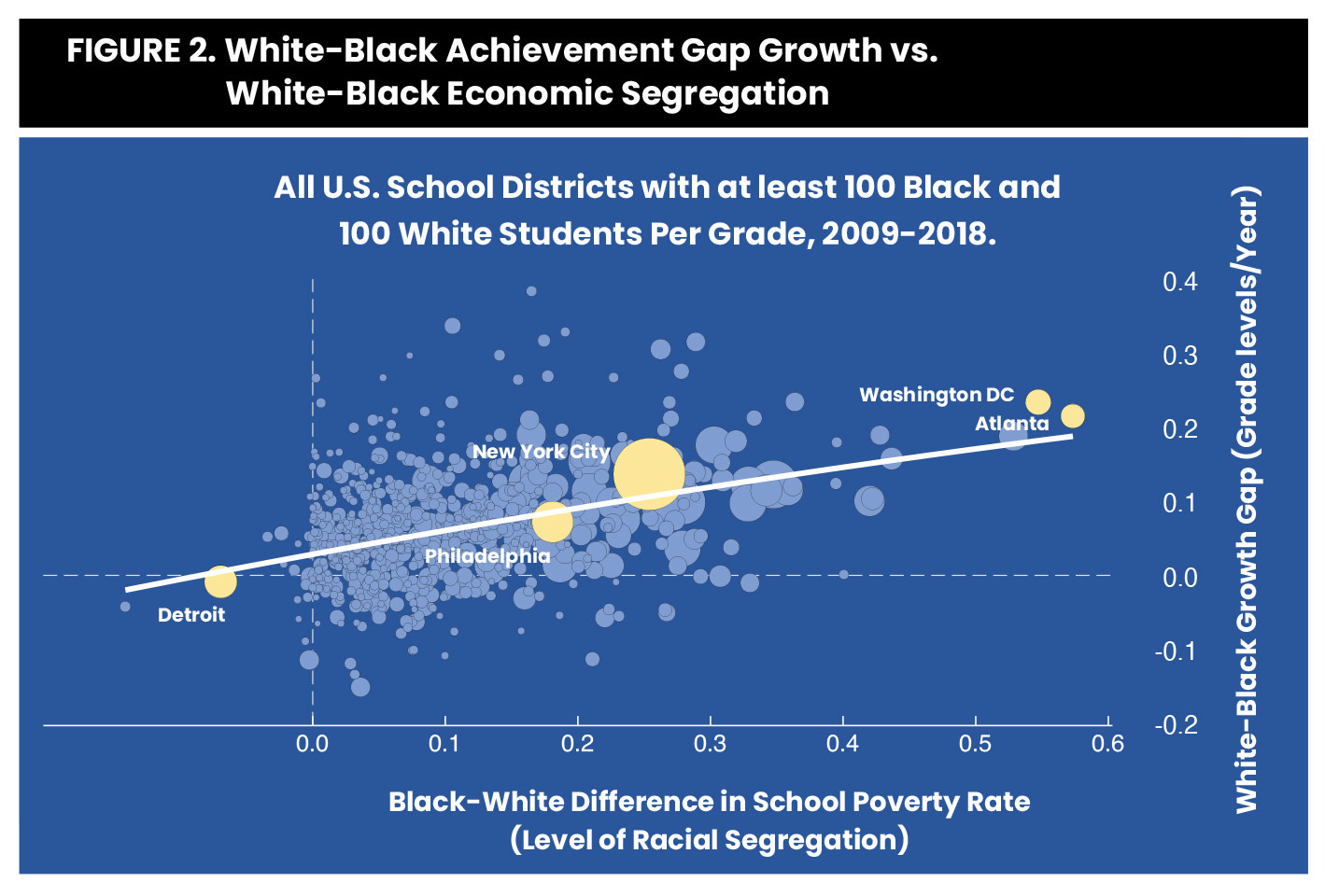 The Future Of School Desegregation In The Wake Of Doj Decision
May 03, 2025
The Future Of School Desegregation In The Wake Of Doj Decision
May 03, 2025
Latest Posts
-
 Peak Solar Power In The Netherlands Utility Trial On Lower Tariffs
May 04, 2025
Peak Solar Power In The Netherlands Utility Trial On Lower Tariffs
May 04, 2025 -
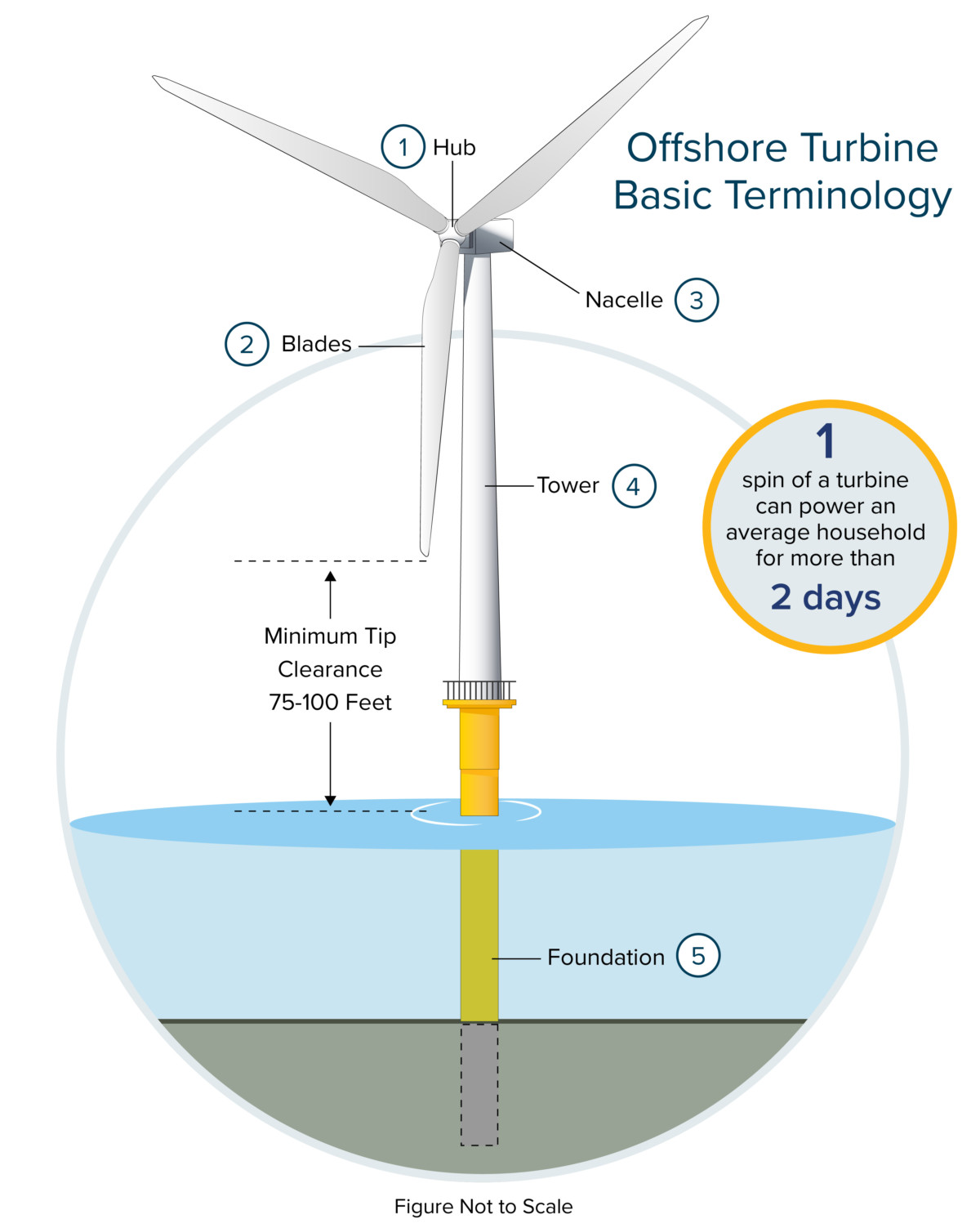 Offshore Wind Farm Economics A Look At The Challenges And Future Outlook
May 04, 2025
Offshore Wind Farm Economics A Look At The Challenges And Future Outlook
May 04, 2025 -
 Innomotics Eneco And Johnson Controls Unveiling A Groundbreaking Heat Pump System
May 04, 2025
Innomotics Eneco And Johnson Controls Unveiling A Groundbreaking Heat Pump System
May 04, 2025 -
 Dutch Solar Power Surplus Experimenting With Dynamic Electricity Pricing
May 04, 2025
Dutch Solar Power Surplus Experimenting With Dynamic Electricity Pricing
May 04, 2025 -
 Are Expensive Offshore Wind Farms Becoming Unviable An Industry Analysis
May 04, 2025
Are Expensive Offshore Wind Farms Becoming Unviable An Industry Analysis
May 04, 2025
