Deadly Fungi: Why The Next Superbug Crisis Will Be Harder To Fight
Table of Contents
The Growing Threat of Antifungal Resistance
Antifungal resistance occurs when fungi develop the ability to survive and even thrive in the presence of antifungal drugs designed to kill them. This resistance develops through various mechanisms, including mutations that alter the drug's target site or the production of enzymes that break down the antifungal medication. The overuse and misuse of antifungals, particularly in healthcare settings, significantly accelerate this process.
Globally, the number of antifungal-resistant infections is steadily increasing. While precise figures are difficult to obtain due to underreporting and variations in surveillance systems, the trend is undeniable. The World Health Organization (WHO) has designated several antifungal-resistant fungi as critical threats, highlighting the urgent need for action.
- Examples of Antifungal-Resistant Fungi: Candida auris, a particularly dangerous fungus, is resistant to multiple antifungal drugs and spreads easily in healthcare facilities. Aspergillus fumigatus, a common mold, is also developing resistance to crucial medications.
- Risk Factors Contributing to Resistance: The widespread use of broad-spectrum antifungals in agriculture and medicine contributes to resistance development. Prolonged hospital stays, especially in intensive care units, expose patients to higher risks of infection and the development of resistance. Immunocompromised individuals are particularly vulnerable.
- Limited Pipeline of New Antifungal Drugs: The development of new antifungal drugs is slow and challenging, leaving us with a limited arsenal to combat resistant strains.
The Unique Challenges of Fighting Fungal Infections
Fungi differ significantly from bacteria, making many antibacterial drugs ineffective. Their eukaryotic cell structure—similar to human cells—makes it incredibly challenging to develop drugs that target fungal cells without harming human cells. This inherent complexity significantly hinders the drug discovery process.
Developing new antifungal drugs is further hampered by the slow growth rate of fungi compared to bacteria, making research and testing considerably more time-consuming and expensive. Additionally, accurate and rapid diagnostic tools for fungal infections are often lacking, delaying treatment and contributing to higher mortality rates.
- Targeting Fungal Cells: The similarity between fungal and human cells means that many potential antifungal drugs also have toxic effects on human tissues.
- Slow Growth Rate: The slow growth rate of fungi makes it difficult to study their biology and develop effective treatments in a timely manner.
- Diagnostic Challenges: The lack of rapid and accurate diagnostic tools often leads to delayed or inappropriate treatment, increasing the risk of mortality and the spread of resistance.
The Impact of Climate Change on Fungal Infections
Climate change significantly impacts the spread and virulence of fungal pathogens. Rising temperatures and increased humidity create more favorable environments for fungal growth and proliferation, expanding the geographic range of many fungal species. This increased prevalence leads to a higher incidence of fungal infections, particularly in immunocompromised individuals.
- Expanding Geographic Ranges: Several fungi, previously confined to specific regions, are now spreading to new areas due to climate change, increasing exposure for populations not previously at risk.
- Increased Incidence in Immunocompromised Individuals: Climate change-related factors, such as increased air pollution and extreme weather events, can weaken immune systems, making individuals more susceptible to fungal infections.
- Increased Exposure to Fungal Spores: Changing weather patterns, including more frequent and intense rainfall, can lead to higher concentrations of fungal spores in the air, increasing exposure and the risk of infection.
Prevention and Public Health Strategies
Preventing the spread of deadly fungi and mitigating the threat of antifungal resistance requires a multifaceted approach focused on infection prevention and control, responsible antifungal use, and robust surveillance systems. Healthcare settings must implement strict infection control protocols, including hand hygiene, environmental cleaning, and appropriate isolation procedures.
- Infection Prevention and Control: Strict adherence to hand hygiene protocols, meticulous environmental cleaning, and appropriate isolation techniques are crucial in healthcare settings.
- Responsible Antifungal Use: Clinicians must use antifungals judiciously, avoiding overuse and ensuring appropriate dosing regimens. Stewardship programs promoting responsible antifungal use are vital.
- Surveillance and Research: Investing in surveillance systems to monitor the emergence and spread of antifungal resistance is essential. Increased research and development of new antifungals and diagnostic tools are crucial for combating this growing threat.
Addressing the Deadly Fungi Threat
The rise of antifungal resistance, coupled with the impacts of climate change, poses a serious threat to global public health. The unique challenges of treating fungal infections demand a collaborative, multi-pronged strategy. Prevention through stringent infection control measures and responsible antifungal use is paramount. Simultaneously, we must significantly increase investment in research and development of new antifungal drugs and diagnostic tools. The future of healthcare depends on our ability to address this looming superbug crisis effectively. We must all work together – learn more about deadly fungi, support relevant research initiatives, and advocate for stronger public health measures to prevent the next global health emergency caused by these deadly fungi. Engage with organizations like the WHO and local public health authorities to contribute to a safer future.
Featured Posts
-
 New Crypto Etfs Trump Media And Crypto Com Partnership Explained
May 08, 2025
New Crypto Etfs Trump Media And Crypto Com Partnership Explained
May 08, 2025 -
 Snegopady V Yaroslavskoy Oblasti Prognoz Pogody I Rekomendatsii
May 08, 2025
Snegopady V Yaroslavskoy Oblasti Prognoz Pogody I Rekomendatsii
May 08, 2025 -
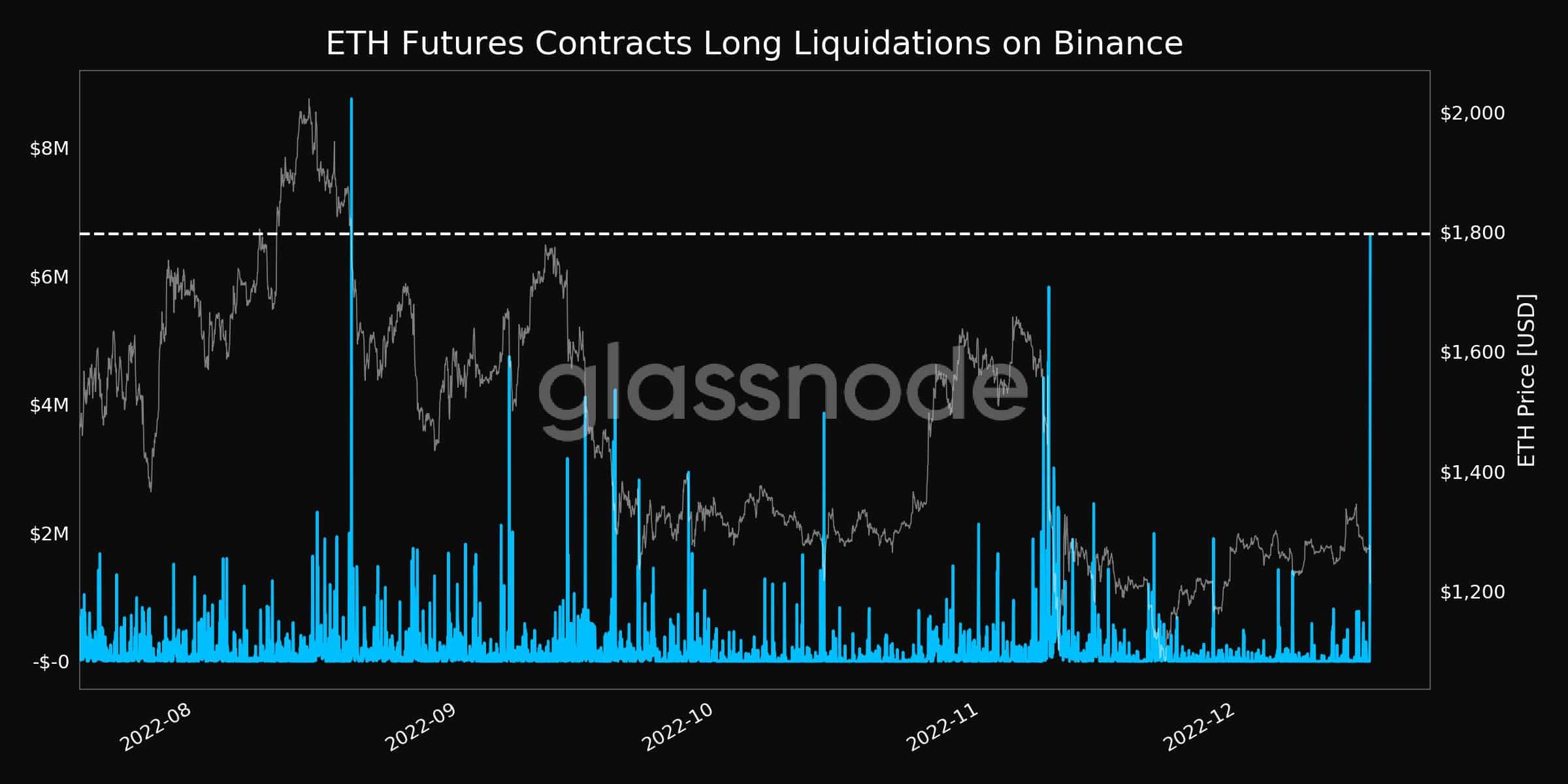 Ethereum Market Crash Recent 67 M Liquidation Raises Concerns
May 08, 2025
Ethereum Market Crash Recent 67 M Liquidation Raises Concerns
May 08, 2025 -
 Taiwans Strengthening Currency Implications For Economic Restructuring
May 08, 2025
Taiwans Strengthening Currency Implications For Economic Restructuring
May 08, 2025 -
 Diego Luna On Andor Season 2 A Departure From Disneys Star Wars Formula
May 08, 2025
Diego Luna On Andor Season 2 A Departure From Disneys Star Wars Formula
May 08, 2025
