Ghana's Mental Health Crisis: A Nation In Need Of Psychiatric Care

Table of Contents
The Extent of the Problem: Prevalence and Statistics
High Prevalence Rates and Underreporting
While precise data on mental health prevalence in Ghana remains limited due to underreporting and a lack of comprehensive epidemiological studies, the reality is likely far more significant than official statistics suggest. The stigma surrounding mental illness often prevents individuals from seeking help or disclosing their struggles.
- Prevalent Mental Health Conditions: Depression, anxiety disorders, schizophrenia, bipolar disorder, and substance abuse disorders are among the most common mental health conditions affecting Ghanaians.
- Limited Data: Suicide rates and hospital admissions related to mental health issues are underreported, hindering accurate assessment of the crisis's true scale. More robust data collection is urgently needed.
The underreporting is largely a consequence of the stigma associated with mental illness and a lack of awareness within the general population. Many individuals suffer in silence, fearing judgment and discrimination.
Socioeconomic Factors Contributing to the Crisis
Poverty, unemployment, lack of education, and pervasive social inequalities significantly contribute to Ghana's mental health crisis. These factors create a perfect storm of stressors that exacerbate existing vulnerabilities and increase the risk of developing mental health problems.
- Poverty and Unemployment: Financial hardship, job insecurity, and lack of opportunities create significant stress and limit access to essential resources, including healthcare.
- Lack of Education: Limited education and awareness about mental health contribute to stigma and hinder help-seeking behavior.
- Social Inequalities: Discrimination based on gender, ethnicity, or other factors can further marginalize vulnerable populations and worsen their mental health outcomes.
Research consistently demonstrates a strong correlation between socioeconomic disadvantage and increased mental health challenges. Addressing these underlying socioeconomic factors is crucial in tackling the crisis effectively.
The Impact on Individuals, Families, and Society
Untreated mental illness has far-reaching consequences for individuals, families, and Ghanaian society as a whole. The human cost is immense, affecting every aspect of life.
- Individual Impact: Reduced quality of life, impaired functioning, and increased risk of suicide are devastating consequences for individuals suffering from untreated mental illness.
- Family Impact: Families often bear the brunt of caring for affected members, facing emotional, financial, and social strain. Family breakdown and strained relationships are common occurrences.
- Societal Impact: Untreated mental illness contributes to reduced productivity, increased crime rates, and a strain on healthcare resources. The overall economic burden is substantial.
Barriers to Accessing Psychiatric Care in Ghana
Lack of Infrastructure and Resources
Ghana faces a significant shortage of psychiatrists, psychologists, mental health facilities, and essential medications. This severely limits access to timely and appropriate care.
- Psychiatrist Shortage: The number of psychiatrists per capita in Ghana is significantly lower than in many other countries, creating a critical shortage of qualified professionals.
- Geographical Disparities: Access to mental healthcare is unevenly distributed, with rural areas and marginalized communities disproportionately affected by a lack of services.
- Inadequate Facilities: Many existing mental health facilities lack the resources, staff, and infrastructure to provide adequate care.
These infrastructural deficiencies exacerbate the already substantial challenges faced by individuals seeking mental health support.
Stigma and Discrimination
Deep-rooted cultural stigma and societal discrimination significantly hinder individuals from seeking help for mental health problems. Fear of judgment, shame, and social exclusion prevents many from disclosing their struggles.
- Misconceptions and Negative Attitudes: Common misconceptions about mental illness, such as attributing it to witchcraft or weakness, perpetuate stigma and discourage help-seeking.
- Impact on Help-Seeking Behavior: Stigma creates a significant barrier to help-seeking, causing delays in treatment and worsening outcomes.
Addressing stigma through education and awareness campaigns is critical to fostering a more supportive and inclusive environment.
Financial Constraints
The high cost of mental healthcare creates a significant barrier for many Ghanaians, making essential services inaccessible to a large segment of the population.
- Financial Burden: The expenses associated with consultations, medications, and hospitalization often place an unbearable financial burden on patients and their families.
- Limited Affordable Options: Affordable and accessible treatment options are severely limited, leaving many with no choice but to forgo necessary care.
Financial assistance programs and affordable treatment options are essential to ensure that mental healthcare is accessible to all, regardless of socioeconomic status.
Potential Solutions and Interventions for Ghana's Mental Health Crisis
Investing in Mental Health Infrastructure
Increased government funding is crucial for developing robust mental healthcare infrastructure, including training programs for mental health professionals and establishing community-based mental health services.
- Funding for Facilities: Investing in the construction and renovation of mental health facilities, ensuring adequate staffing and equipment.
- Training Programs: Expanding training programs for psychiatrists, psychologists, nurses, and other mental health professionals to meet the growing demand for qualified personnel.
- Community-Based Services: Developing and implementing community-based mental health programs that provide accessible and culturally appropriate services.
Addressing Stigma Through Public Awareness Campaigns
Raising public awareness about mental health, promoting understanding, and combating stigma are essential to encourage help-seeking behavior and foster a supportive environment.
- Educational Programs: Developing and implementing comprehensive educational programs in schools, workplaces, and communities to promote mental health literacy.
- Media Campaigns: Utilizing media platforms to raise awareness, challenge stigma, and promote positive representations of mental health.
- Community Engagement: Engaging community leaders, religious organizations, and traditional healers to promote understanding and reduce stigma.
Integrating Mental Health into Primary Healthcare
Integrating mental health services into primary care settings can significantly improve accessibility and early intervention, particularly in rural areas with limited specialized mental health resources.
- Training Primary Care Providers: Equipping primary care providers with the skills and knowledge to screen for and manage common mental health conditions.
- Referral Pathways: Establishing clear referral pathways between primary care and specialized mental health services.
- Collaborative Care Models: Implementing collaborative care models that involve primary care physicians, mental health professionals, and other healthcare providers working together to provide comprehensive care.
Training and Capacity Building
Training and capacity building are critical to expanding the mental health workforce and improving the quality of care provided.
- University Partnerships: Strengthening partnerships between universities and healthcare institutions to provide training opportunities for mental health professionals.
- Continuing Professional Development: Offering continuing professional development opportunities to update the knowledge and skills of existing mental health professionals.
- Mentorship Programs: Establishing mentorship programs to support the professional development of newly trained mental health professionals.
Conclusion
Ghana's mental health crisis demands urgent and comprehensive action. The lack of resources, pervasive stigma, and socioeconomic factors combine to create significant barriers to accessing psychiatric care for millions of Ghanaians. Addressing this crisis requires a multifaceted approach encompassing increased investment in mental health infrastructure, comprehensive public awareness campaigns to combat stigma, and the integration of mental healthcare into primary care settings. We must also prioritize training and capacity building to ensure a sufficient number of qualified mental health professionals. Let's work together to ensure that every Ghanaian has access to the psychiatric care they need, fostering a healthier and more equitable society.

Featured Posts
-
 Is Beijing Hiding The True Cost Of The Trade War With America
May 02, 2025
Is Beijing Hiding The True Cost Of The Trade War With America
May 02, 2025 -
 Popular Indigenous Arts Festival Under Threat From Economic Crisis
May 02, 2025
Popular Indigenous Arts Festival Under Threat From Economic Crisis
May 02, 2025 -
 Tuerkiye De 1 Mayis Emek Ve Dayanisma Guenue Gecmisten Guenuemueze Bir Bakis
May 02, 2025
Tuerkiye De 1 Mayis Emek Ve Dayanisma Guenue Gecmisten Guenuemueze Bir Bakis
May 02, 2025 -
 30 Shkhsyt Mn Akthr Allaebyn Walmdrbyn Krha Fy Tarykh Krt Alqdm Mwqe Bkra
May 02, 2025
30 Shkhsyt Mn Akthr Allaebyn Walmdrbyn Krha Fy Tarykh Krt Alqdm Mwqe Bkra
May 02, 2025 -
 Kycklingnuggets Med Majsflingor Krispiga And Goda Med Asiatisk Kalsallad
May 02, 2025
Kycklingnuggets Med Majsflingor Krispiga And Goda Med Asiatisk Kalsallad
May 02, 2025
Latest Posts
-
 L Implication De Macron Dans Le Choix Du Futur Pape Analyse Des Rumeurs De Rome
May 03, 2025
L Implication De Macron Dans Le Choix Du Futur Pape Analyse Des Rumeurs De Rome
May 03, 2025 -
 Macron Au Gabon La Fin De La Francafrique
May 03, 2025
Macron Au Gabon La Fin De La Francafrique
May 03, 2025 -
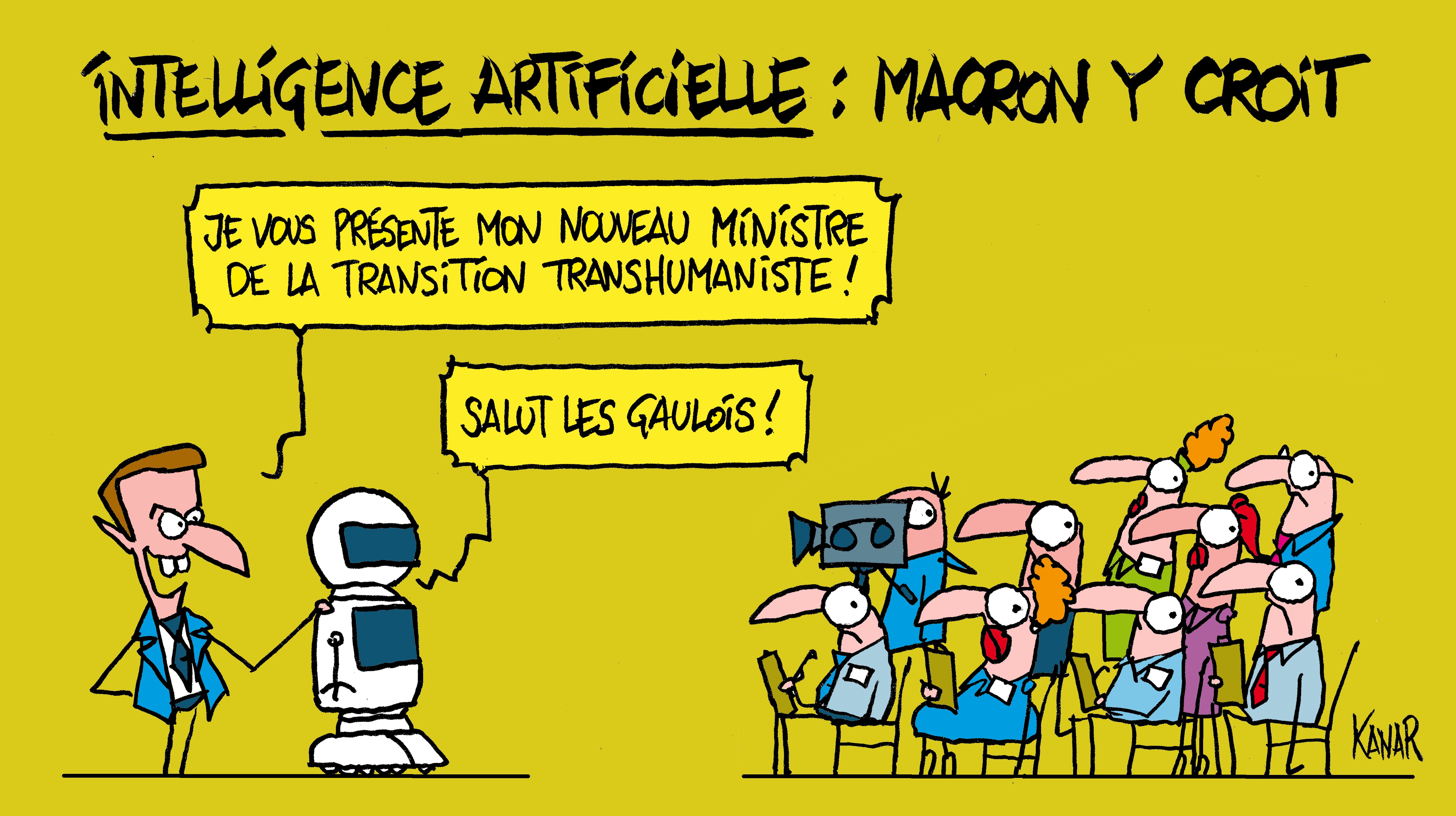 Intelligence Artificielle Macron Et Le Patriotisme Economique Europeen
May 03, 2025
Intelligence Artificielle Macron Et Le Patriotisme Economique Europeen
May 03, 2025 -
 Rome L Ombre De Macron Sur Le Prochain Conclave
May 03, 2025
Rome L Ombre De Macron Sur Le Prochain Conclave
May 03, 2025 -
 La Francafrique Macron Annonce Une Nouvelle Ere Au Gabon
May 03, 2025
La Francafrique Macron Annonce Une Nouvelle Ere Au Gabon
May 03, 2025
